| disease | Alcoholic Hepatitis |
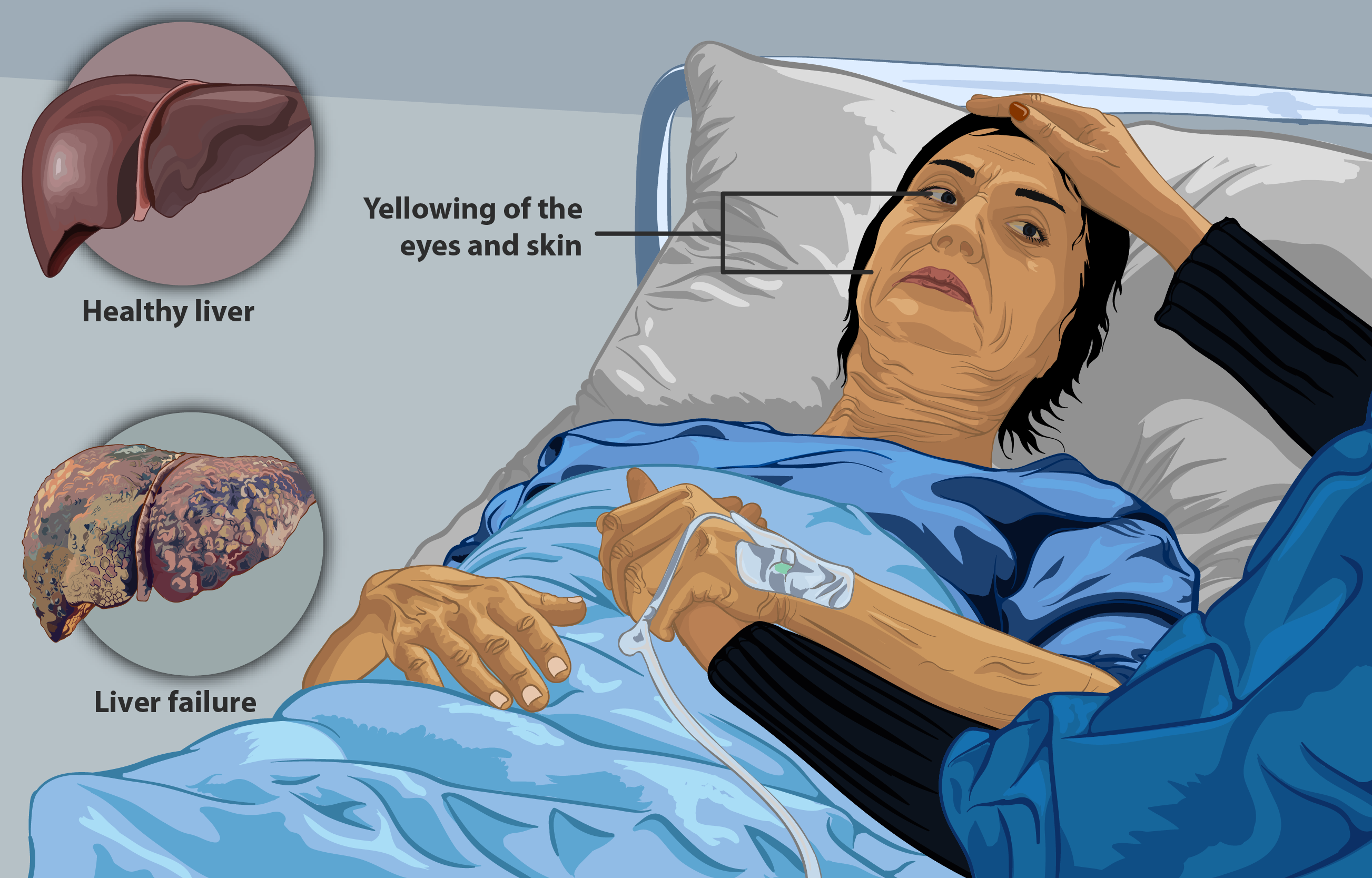
| summary | Alcoholic hepatitis is a serious liver inflammation primarily caused by excessive alcohol consumption. It's characterized by liver cell damage and inflammation, potentially leading to liver failure if untreated. |
| name | Alcoholic Hepatitis |
| type | Liver disease |
| classification | Inflammatory condition, potentially acute or chronic. |
| symptoms | | 1 | Abdominal pain (often in the upper right quadrant) | | 2 | Fever | | 3 | Fatigue | | 4 | Loss of appetite | | 5 | Nausea and vomiting | | 6 | Jaundice (yellowing of the skin and eyes) | | 7 | Ascites (fluid buildup in the abdomen) | | 8 | Encephalopathy (confusion, altered mental status) |
|
| signs | | 1 | Hepatosplenomegaly (enlarged liver and spleen) | | 2 | Jaundice | | 3 | Ascites | | 4 | Peripheral edema | | 5 | Asterixis (flapping tremor) | | 6 | Changes in mental status | | 7 | Abdominal tenderness | | 8 | Bruising or bleeding tendency |
|
| causes | Excessive and prolonged alcohol consumption. |
| detailed etiology pathogenesis | Chronic alcohol abuse leads to the accumulation of toxic metabolites, primarily acetaldehyde, which directly damage liver cells (hepatocytes). This damage triggers an inflammatory response. Free radicals, oxidative stress, and immune system activation further contribute to the inflammatory process and liver cell injury. Fatty liver (steatosis) is frequently a precursor to alcoholic hepatitis. The inflammatory response can lead to liver fibrosis and cirrhosis if the condition persists. |
| investigations | | 1 | Complete blood count (CBC) | | 2 | Liver function tests (LFTs): ALT, AST, bilirubin, albumin, prothrombin time (PT) | | 3 | Coagulation studies | | 4 | Serum creatinine and electrolytes | | 5 | Blood alcohol level (BAL) (though not always done for diagnosis) | | 6 | Imaging studies (ultrasound, CT scan, MRI): To assess the extent of liver damage, look for complications like ascites. | | 7 | Liver biopsy: Gold standard for definitive diagnosis, especially to assess the degree of inflammation, fibrosis, and necrosis. |
|
| treatment options | | 1 | Discontinue alcohol consumption immediately. | | 2 | Supportive care (rest, adequate nutrition): Focus on hydration and nutritional support. | | 3 | Medical therapies: Corticosteroids (prednisolone) are sometimes used to reduce inflammation, but evidence suggests limited benefit and significant risks. | | 4 | Nutritional support (vitamins, minerals): Important to address nutritional deficiencies, often associated with alcoholism. | | 5 | Management of complications: Ascites, encephalopathy, and bleeding require specific interventions. | | 6 | Liver transplantation: Considered for severe cases with end-stage liver disease. |
|
| differentials | | 1 | Viral hepatitis (A, B, C, D, E) | | 2 | Autoimmune hepatitis | | 3 | Nonalcoholic fatty liver disease (NAFLD) | | 4 | Other liver diseases | | 5 | Drug-induced liver injury |
|
| prevention | Abstaining from excessive alcohol consumption is the primary preventive measure. |
| prognosis | Prognosis varies depending on the severity of the condition and response to treatment. Early diagnosis and intervention improve outcomes. Patients with severe alcoholic hepatitis, particularly with complications, have a poor prognosis. |
| other important details | | 1 | Severity can range from mild to life-threatening. Prompt intervention is crucial in severe cases to prevent liver failure and other complications. | | 2 | Often co-exists with other alcohol-related health problems. | | 3 | Alcohol-related liver disease (ARLD) encompasses a spectrum of conditions, including fatty liver, alcoholic hepatitis, and cirrhosis. |
|