| name | Omalizumab |
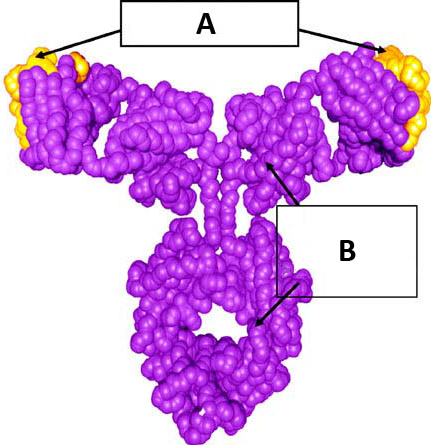
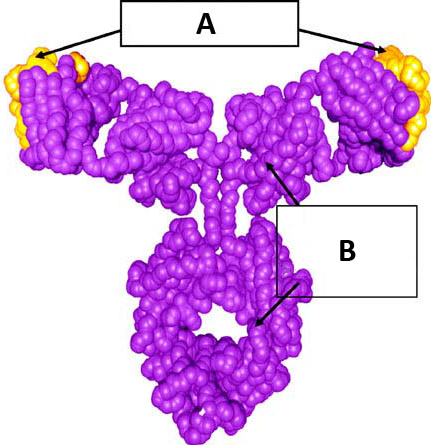
| classification | Monoclonal antibody, anti-IgE |
| pharmacokinetics | | absorption | Subcutaneous injection; Absorption is rapid. | | distribution | Distributes to tissues and organs; Primarily bound to serum proteins. | | metabolism | Metabolized in the liver; primarily eliminated unchanged in the urine. | | elimination | Elimination half-life is approximately 2 weeks to several months. Elimination primarily through renal excretion. |
|
| suggested dosage | | notes | Dosage varies greatly based on patient factors (e.g., severity of allergic disease, body weight) and must be determined and monitored by a healthcare professional. | | initial dose | Individualized based on clinical factors. Typically administered over 16 weeks to achieve the desired target serum omalizumab level. | | maintenance dose | Administered every 2-4 weeks. | | weight specific considerations | Dosage is often adjusted based on body weight. This data is specific to a 70 kg individual; a physician should adjust according to the patient's specifics. |
|
| indications | | 1 | Moderate to severe persistent allergic asthma not controlled by inhaled corticosteroids and other controller medications, particularly in patients with elevated serum IgE levels. | | 2 | Urticaria and chronic idiopathic urticaria. | | 3 | Severe allergic reactions (anaphylaxis). |
|
| safety in pregnancy | | details | Limited data on pregnant women. Available information suggests omalizumab does not cross the placenta in high amounts, so the risk of harm to the fetus is considered low. | | recommendations | Omalizumab should be used during pregnancy only if clearly needed and under the close supervision of a specialist with experience in both pregnancy and allergic diseases. Regular monitoring of mother and fetus is essential. | | category | Category B (based on animal studies. No adequate and well-controlled studies in pregnant women.) |
|
| safety in breastfeeding | | details | Limited information on breastfeeding mothers. Omalizumab is not known to be secreted in breast milk in significant amounts, suggesting a potentially low risk of harm to a nursing infant. | | recommendations | Omalizumab use during breastfeeding should be carefully considered, and the risk/benefit should be evaluated on a case-by-case basis with close monitoring of the infant. | | category | Category unknown. |
|
| side effects | | 1 | Injection site reactions (pain, redness, swelling) | | 2 | Headache | | 3 | Nasopharyngitis (common cold symptoms) | | 4 | Fatigue | | 5 | Upper respiratory tract infections | | 6 | Urticaria | | 7 | Serious adverse events: anaphylaxis, hypersensitivity reactions, including angioedema and bronchospasm. | | 8 | Rare cases of infections (bacterial, viral, fungal) and other complications have been reported. |
|
| alternatives | |
| contraindications | | 1 | Hypersensitivity to omalizumab or any of its components. | | 2 | History of severe allergic reactions to medications (important to disclose to physician). |
|
| interactions | | 1 | Potential interaction with other medications affecting liver or kidney function. (Important to disclose to physician all current medications). |
|
| warnings and precautions | | 1 | Careful monitoring is essential for patients with a history of allergic reactions or asthma attacks. | | 2 | Advise patients of potential injection site reactions and other potential side effects. | | 3 | Ensure proper injection technique is followed to minimize the risk of complications. | | 4 | Dosage and frequency should be managed by the prescriber only and must be followed exactly to prevent severe adverse reactions. |
|
| additional informations | | mechanism of action | Omalizumab binds to free IgE in the serum, preventing IgE from binding to mast cells and basophils. This reduces the release of inflammatory mediators and allergic reactions. |
|
| patient specific notes | | age | 25 | | weight | 70 kg | | additional patient info | Further information or a complete medical history is needed to determine suitable dosage and whether the drug is appropriate for this patient. |
|